Shifting Sites of Patient Care: Driving Value in Alternative Settings
Right care, right setting: Unlocking value in alternative sites of care

A century ago, house calls were the standard for healthcare. Doctors would come directly to the patient’s doorstep, black bag in hand, to treat everything from minor ailments to serious conditions.
Today, that model is coming back in a major way—driven by technology, consumer preferences, hospital capacity shortages, new payment models and favorable regulations. As healthcare delivery shifts from traditional sites to lower-cost settings like homes, telehealth and retail locations, care is ultimately moving closer to patients themselves.
That’s good news for payers, providers and patients alike. These “alternative sites of care” can improve care access, quality and continuity while reducing healthcare spend. That’s why we’re building companies that leverage alternative care settings—one of our focus areas for 2023. For instance, MedArrive, a company built at Redesign Health, delivers community-based, in-home care, so patients get the medical attention they need without visiting a hospital. We’re also partnering with a leading health system to build a new company that will offer cardiac rehab in the comfort of patients’ homes, including a personalized care plan and dedicated coach.
Right care, right setting
Despite the benefits of alternative sites of care, it’s not enough to move care closer to the patient. Health systems and other providers must deliver care in the most appropriate setting, based on a multitude of factors. As such, site-of-care optimization has become an important tool to manage healthcare spend, utilization and delivery. This approach is gaining widespread adoption among providers, payers and government stakeholders.
At Redesign Health, we see a variety of opportunities to help these stakeholders:
Leverage technology, such as remote patient monitoring, to transition patients into the right care setting
Upskill health care practitioners to better practice at the top of their licenses in certain settings
Improve the quality of medical and non-medical care received outside inpatient settings
Experts across the Redesign Health ecosystem shared their insights into five key considerations for driving clinical and financial value across alternative sites of care:
1. Enabling preventive, proactive care
Redesign Health has built several companies that support alternate sites of care; most of them focus on opportunities to optimize and shift sites of care along the acute and post-acute spectrum. But site-of-care optimization plays a key role in preventive care and ongoing wellness activities, too.
Preventive care begins with regular primary care provider (PCP) visits, but medical, behavioral or social challenges can prevent patients from receiving this type of care. Strengthening the patient-PCP relationship is the first major step toward shifting care from a reactive model to a proactive one.
“Site-of-care optimization can play a huge role in a patient’s long-term wellness,” says Dan Trigub, co-founder and CEO at MedArrive, which leverages a network of trusted EMS providers who act as a bridge between patient and physician, providing medical support to patients when and where they need it. “Patients are more likely to accept care when they can receive it in a comfortable, accessible setting. And once a patient is empowered by receiving care in their home, care providers can assist in reconnecting them with a PCP.”
2. Engaging other stakeholders as champions and supports
Multiple stakeholders are involved in alternative care settings, notes Ugo Uwaoma, CEO of a stealth company built at Redesign Health, which reimagines the patient care continuum and enables more effective patient transitions by leveraging alternative sites of care. This includes:
Family: “Transitions to alternative care sites bring unique challenges with communication and support,” Uwaoma says. “Engaging the family support team is key to success for most patients, especially those who are elderly.”
Caregivers: “Clinicians, social workers and care managers are dealing with burnout caused by inadequate staffing and clinical overwhelm,” Uwaoma notes. “We should prioritize any opportunity to maximize care sites that lead to people working at the top of their licenses or reduce staff burden.”
Businesses and communities: “Employers, community organizations, churches and social agencies must be engaged in supporting patients to ensure sustainable care optimization,” says Uwaoma.
Fostering a strong support network for patients is key, Uwaoma notes. “We have to understand what a day in their life is like, then make a plan to support their needs,” he says. “We can align with community leaders and jointly partner to meet the broader needs of the community, engaging community members to help translate context and improve effectiveness. Be there for the long term and trust is earned over time.”
3. Driving health equity by meeting patients where they are
The ability to engage hard-to-reach populations is a major advantage of alternative sites of care. But to achieve this advantage, programs must be designed with intention, based on the needs of that patient population.
During the pandemic, Reza Alavi, a Redesign Health Advisor and Former Chief Clinical Officer at DispatchHealth, saw firsthand how patients were grateful to receive on-demand, home-based care. This experience guides his views on themes that help underserved populations to accept care.
“We’re guests in the patient’s homes and should act accordingly,” Alavi says. “We should engage acutely symptomatic patients from the very first visit, rather than initiating interactions through routine transition of care or health risk assessment. And we must provide the exact same high-quality product to all, without allowing reimbursement margin pressure to water down interventions.”
In the case of MedArrive, its field providers are paramedics and EMTs who are already staples of the local community. These providers have years of experience treating patients at their most vulnerable moments. They use plain, accessible language to help patients feel at ease and empowered during the care experience.
“Earning a patient’s trust and comfort is an honor that should not be taken lightly,” says Dan Trigub of MedArrive. “Every point of contact with patients is an opportunity to create a warm, welcoming experience. Each patient should feel like their care is personalized and provided for their benefit.”
4. Improving access to data to inform care settings
To be able to determine the best setting of care, stakeholders must understand not only the physiological state of a patient but also the social and behavioral challenges that can impact a patient’s health. One barrier to innovation has been the fact that stakeholders have traditionally only had access to one cut of the larger data picture.
“Payers often consider site-of-care optimization informed by limited data sources like admission, discharge, and transfer (ADT) or claims data, whereas providers often leverage their point-of-care health data to make these determinations,” says Dan Trigub. “When a patient is lost to follow-up, hasn’t seen their primary care provider in a long time, or can’t access care until they have an emergent event, payers and providers may have close to no data on that patient.”
Without a whole-person view, healthcare organizations can’t leverage tangible data to understand cost and patient experience implications. All healthcare stakeholders stand to benefit from patient engagement and outreach teams that can “be their eyes.”
5. Leveraging a favorable regulatory environment
The government as a payer has also supported site-of-care optimization—particularly because innovations in technology and clinical care have reduced the risk of catastrophic complication for many procedures. Now, CMS has enabled Medicare reimbursement in outpatient settings (such as ambulatory service centers) for many procedures that were previously considered inpatient-only.
Final thoughts
As adoption of alternative care settings continues to grow, so will the opportunities to build new, impactful solutions.
“Risk-bearing entities will incrementally shift leadership bandwidth and resources on the delivery of right care, right time, right place at scale,” predicts Reza Alavi. “In addition to improving access to primary care, a portfolio of new solutions will be needed to optimize value-based outcomes in other transition points, such as emergency rooms, obstetrics, inpatient care and skilled nursing facilities.”
We are optimistic about the many opportunities in this space to deliver better care, and are focused on funding and launching companies that optimize care delivery, benefiting patients and other healthcare stakeholders alike.
![No alternate text]() Redesign HealthDemystifying Healthcare Innovation: 4 Lessons on Driving Meaningful Change
Redesign HealthDemystifying Healthcare Innovation: 4 Lessons on Driving Meaningful ChangeInnovation is a frequently used buzzword in healthcare. Despite its widespread usage within our industry, achieving tangible value and impactful outcomes often proves challenging.
April 16, 2024
![No alternate text]() Healthcare TrendsRedesign Health2024 Health Trends: 4 Experts Discuss Key Innovation Priorities
Healthcare TrendsRedesign Health2024 Health Trends: 4 Experts Discuss Key Innovation PrioritiesTo uncover the most pressing healthcare issues—and possible solutions—on the horizon for 2024, our team polled four influential industry thought leaders and Executive Advisory Board members at Redesign Health.
January 10, 2024
![No alternate text]() MedicaidModernizing Medicaid with a Multi-Stakeholder Financing Model
MedicaidModernizing Medicaid with a Multi-Stakeholder Financing ModelDiscover how a multi-stakeholder financing model could overcome some of Medicaid’s obstacles, dramatically improving health and quality of life outcomes for Medicaid recipients while generating savings across government programs.
November 15, 2023
![No alternate text]() Chronic CareRedesign HealthWraparound Care: The Next Frontier in Chronic Care Management
Chronic CareRedesign HealthWraparound Care: The Next Frontier in Chronic Care ManagementExploring tech-infused strategies to manage chronic conditions
September 05, 2023
![No alternate text]() ADVISORSRedesign HealthRedesign Health Advise: Leveraging Experts and Insights to Expand Impact
ADVISORSRedesign HealthRedesign Health Advise: Leveraging Experts and Insights to Expand ImpactThe Redesign Health Advise program connects our team and founders with a deep bench of experts from across the healthcare industry.
June 29, 2023
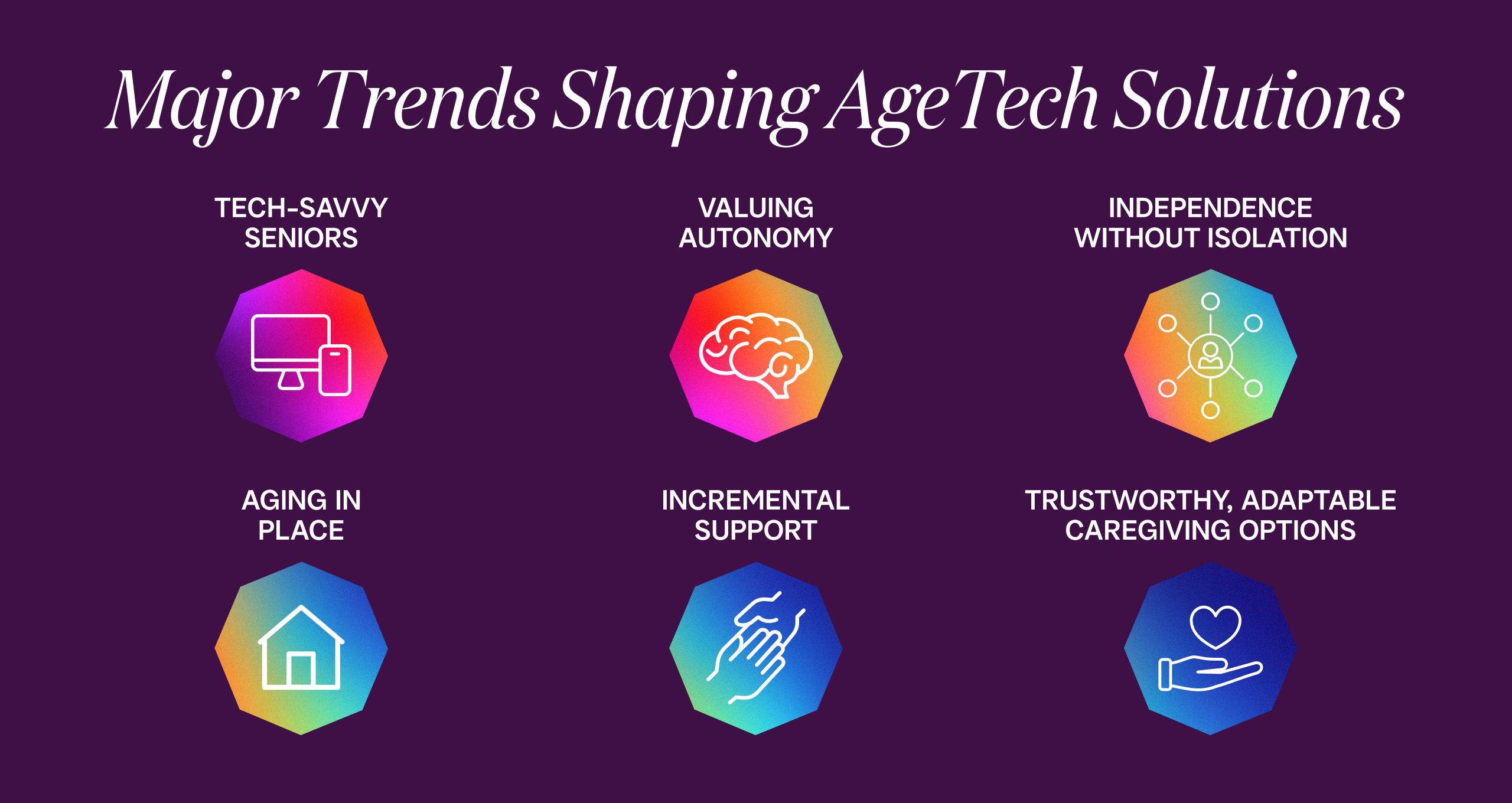
![No alternate text]() Senior HealthRedesign HealthInvesting in AgeTech: Serving the Growing Senior Health Market
Senior HealthRedesign HealthInvesting in AgeTech: Serving the Growing Senior Health MarketProviding targeted tech solutions for aging adults
June 14, 2023
![No alternate text]() Shifting Sites of Patient Care: Driving Value in Alternative Settings
Shifting Sites of Patient Care: Driving Value in Alternative SettingsRight care, right setting: Unlocking value in alternative sites of care
April 27, 2023
![No alternate text]() Value-Based CareThe Evolution of Value-Based Care: Exploring Challenges and Opportunities in Adoption
Value-Based CareThe Evolution of Value-Based Care: Exploring Challenges and Opportunities in AdoptionRedesign Health Venture Chair Missy Krasner recently hosted a roundtable discussion with leaders in the Value-Based Care Industry to explore how the adoption of value-based care is unfolding--and what to expect in the coming years.
February 15, 2023
![No alternate text]() James QuarlesThe Kids Aren’t Alright: Addressing the Adolescent Mental Health Crisis With Accessible, High Quality, Evidence-Based Practice
James QuarlesThe Kids Aren’t Alright: Addressing the Adolescent Mental Health Crisis With Accessible, High Quality, Evidence-Based PracticeResearch shows that mental health disorders have surpassed physical conditions as the most common causes of impairments and limitations in children. Suicide was the second-leading cause of death among 10 to 14 year-olds in 2020.
February 15, 2023
![No alternate text]() PartnershipsRedesign HealthPartnering with Leading Health Systems to Drive Change and Improve Outcomes
PartnershipsRedesign HealthPartnering with Leading Health Systems to Drive Change and Improve OutcomesAt Redesign Health, we firmly believe the US healthcare system desperately needs innovation to address our lagging health outcomes, sky-high costs and uneven access to care.
February 09, 2023
![No alternate text]() Platform, Company CreationBehind the Curtain: Redesign Health's Company Creation Process
Platform, Company CreationBehind the Curtain: Redesign Health's Company Creation ProcessIt's easy to say healthcare is broken. It's much harder to fix it. At Redesign Health, we’re up for the challenge.
February 01, 2023
![No alternate text]() Healthcare TrendsHealthcare’s Biggest Trends in 2023: Industry Forecast from Redesign Health
Healthcare TrendsHealthcare’s Biggest Trends in 2023: Industry Forecast from Redesign HealthPowering healthcare innovation at scale is the heart of our work at Redesign Health. With 2023 on the horizon, we surveyed our cross-functional team of industry leaders for their forecast for 2023’s biggest trends in healthcare.
December 15, 2022
![No alternate text]() Insights from the Redesign Health Ecosystem: Improving Healthcare for Older Adults
Insights from the Redesign Health Ecosystem: Improving Healthcare for Older AdultsRedesign Health Venture Chair Missy Krasner recently hosted a roundtable discussion with leaders from three of our Operating Companies to explore the state of older adult healthcare in the U.S. and how their teams are facilitating healthier aging.
October 21, 2022
![No alternate text]() ResearchRedesign HealthStuck in the Middle: Healthcare Solutions for Older Adults Shouldn’t Be One Size Fits All. Here's Why.
ResearchRedesign HealthStuck in the Middle: Healthcare Solutions for Older Adults Shouldn’t Be One Size Fits All. Here's Why.There will be more older adults than children in America by 2035. We are not ready. A one-size-fits-all approach to older adult healthcare simply won’t be able to comprehensively support the needs of so many aging people.
October 05, 2022
![No alternate text]() Company CultureRedesigning Company Culture
Company CultureRedesigning Company CultureWe have big ambitions at Redesign Health: to make humanity healthier and to redesign healthcare for everyone. We strive to do things differently here, and building our company culture is no exception.
July 18, 2022